Fracture Below Previous Lumbar Stabilization System - Second Case
A 73-year-old female patient was brought in with complaints of low back and right leg pain. The patient, who showed signs of dementia, described pain that had been present for several months but had suddenly increased 10 days ago. It was learned that the patient had undergone lumbar stabilization for an L1 fracture in 2018. Her neurological examination was normal apart from the signs of dementia.
The patient had plain radiographs taken one month prior. CT and MRI scans revealed a new fracture at the L4 vertebra, spinal canal stenosis at this level, and a previous cemented transpedicular screw system spanning T11-L3.
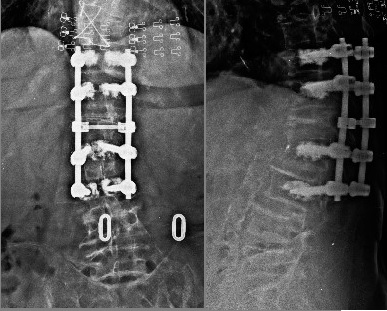
Figure 1: The patient's plain radiographs from one month ago show the previous cemented T11-L3 transpedicular screw system. Irregularity consistent with a fracture is visible on the upper endplate of the L4 body.
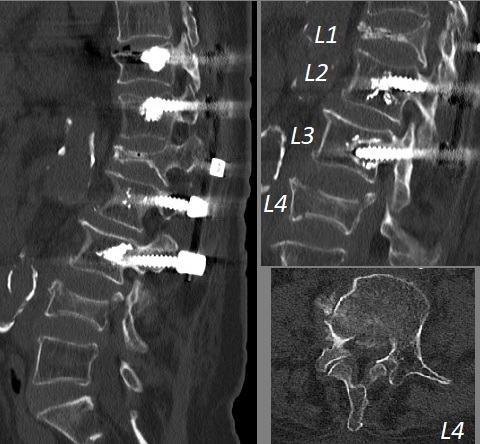
Figure 2: The CT scan shows that the height loss in the L4 vertebra has significantly increased compared to the plain radiograph from a month ago. A bone fragment narrowing the canal is present at this level. While there are signs of mild loosening in the lowest screws (L3) of the cemented system placed for the previous L1 fracture, the system appears functional.
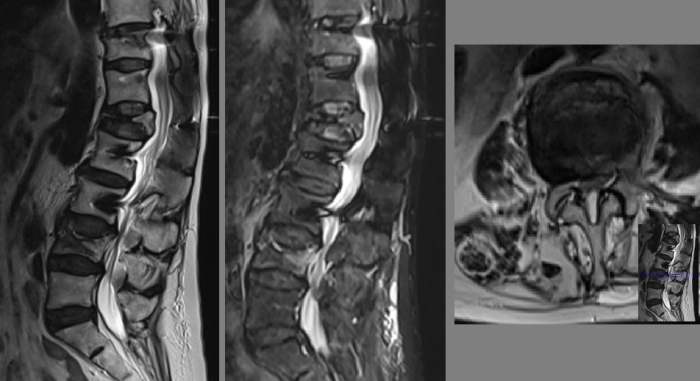
Figure 3: MRI examination reveals an image consistent with an acute/subacute fracture in the L4 vertebra.
A DEXA scan performed a year ago showed a lumbar T-score of -3.2 (osteoporosis). Evaluating her current condition with radiographs and examination findings, vertebroplasty under local anesthesia and sedation was recommended for the progressing L4 fracture, along with an epidural injection for pain relief. It was stated that if the leg pain did not resolve after this procedure, a lumbar decompression surgery might be necessary for the canal stenosis.
Two months after this consultation, the patient was brought back in a wheelchair. From her history, it was learned that after our previous examination, the patient applied to another surgeon and underwent stabilization surgery. However, her pain continued to increase after this operation.
The patient was sitting bent over in a forced posture, experiencing severe leg pain that worsened with slight movements, and was unable to stand up. Although a full examination could not be performed due to pain and dementia, loss of muscle strength was detected in dorsal flexion of both feet.
Her repeated radiological examinations are shown below.
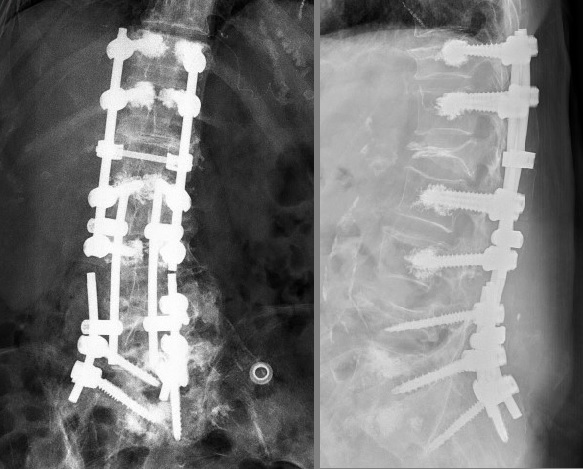
Figure 4: The plain radiograph shows that one screw was placed in the L4 vertebra, and two screws each in the L5 and S1 levels, connecting this system to the previous rod system with dominos. The L5 screws are directed inferiorly (malposition). One of the S1 screws is not visible on the lateral radiograph. Cement is present in the L5 and S1 bodies.
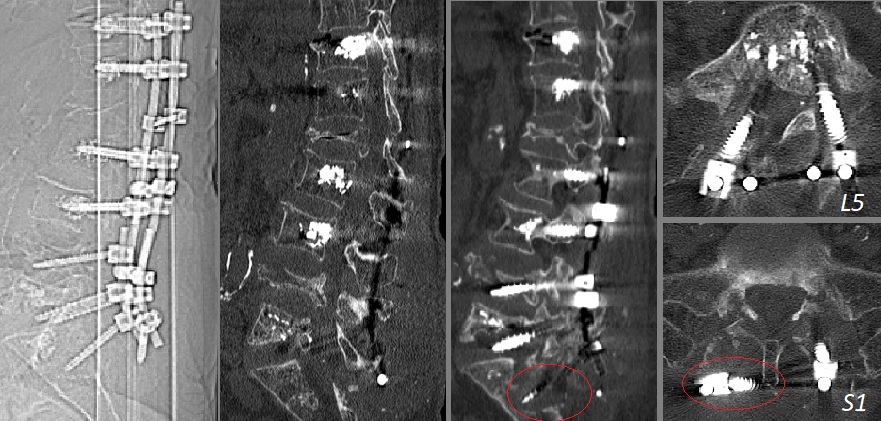
Figure 5: The CT scan shows that both L5 screws are directed inferiorly, with the right one also going medially. They enter the L5-S1 neural foramen on both sides and the canal on the right. The S1 screws have loosened, creating deep cavities in the S1-S2 bodies, and on the right, the S1 screw has completely rotated on the rod and extended to the opposite side. The L4 body has completely lost its height.
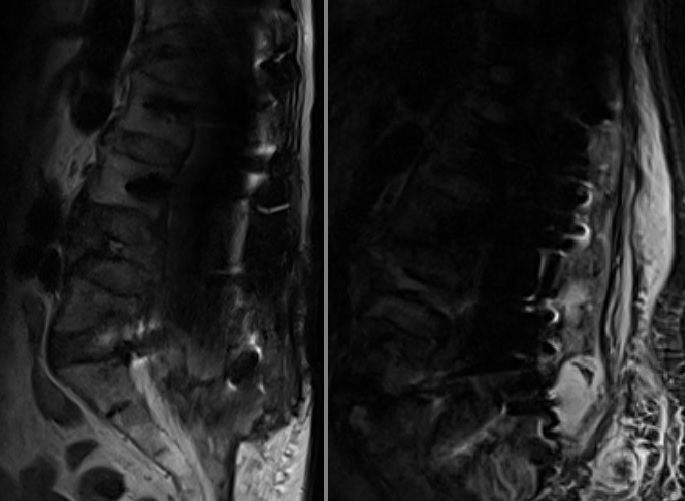
Figure 6: Intense metal artifact makes MRI evaluation impossible. There is a diffuse fluid appearance in the sacral region (hematoma? CSF?).
The patient and her relatives were informed about the current situation. It was explained that the pre-existing problems of L4 vertebral height loss and canal stenosis persisted. Additionally, an instability problem was added at the L5-S1 level, where the facets were damaged due to screw malposition. It was also explained that the screw malpositions were compressing the nerve roots and likely the dural sac.
Since there was no suitable place for transpedicular screw stabilization at the L4, L5, S1, and S2 levels, a stabilization attempt would be useless. It was considered that the only reasonable solution for now would be the removal of all added screws, followed by neural decompression where necessary, then posterior in-situ fusion over the facets and transverse processes using iliac autografts, and strict bed rest in a cast for 3 months. It was stated that after 3-6 months, following bone healing in the area, a new stabilization surgery could be planned if necessary.
The patient's relatives have not yet applied for treatment after this consultation.
CONCLUSION and COMMENT
This case is quite similar to our case from a month ago. In our July case, we strengthened the L4 fracture with vertebroplasty and applied an epidural injection for leg pain. In this patient, the treating surgeon aimed to provide stabilization with instrumentation by extending to intact levels instead of strengthening the fractured vertebra with vertebroplasty. Since it is also possible to provide canal decompression with laminectomy in the same session, this approach may have advantageous aspects. However, this approach is quite risky for a patient with osteoporosis, even without the current bone mineral density data at hand. Descending to the sacrum was not correct. It can easily be predicted that sacral stabilization, which is problematic even in patients with normal bone mineral density, would fail in this patient. As a result, the entire system loosened, and malpositioned screws caused radicular pain.
Stabilization in this patient might have been achieved with ideally placed cemented L5 screws and additionally strengthening the inside of the L4 body with cement, perhaps with a shorter construct or a longer system extending to the iliac bones. Even if done ideally in this way, the risk of implant loosening is still high. In our opinion, in such cases, minimally invasive procedures aimed at controlling pain and stabilizing the collapsing vertebra should be prioritized, and stabilization surgeries should be reserved as a last resort when no other treatment works.