Fracture Below Previous Lumbar Stabilization System
A 60-year-old female patient was brought in a wheelchair with complaints of low back and leg pain. It was learned that her pain had intensified following a fall a month ago and did not decrease despite the medication she used.
It was learned that the patient had undergone stabilization surgery after a fracture was detected in her lower back following a fall in 2015, had intermittent low back pain that increased over the last year, and also had sequelae left spastic hemiparesis after a disease in childhood.
MRI examination showed a new fracture in the L4 vertebra. Plain radiograph and CT examinations revealed that the previously performed T11-L3 stabilization system had loosened at the lower end and become dysfunctional.
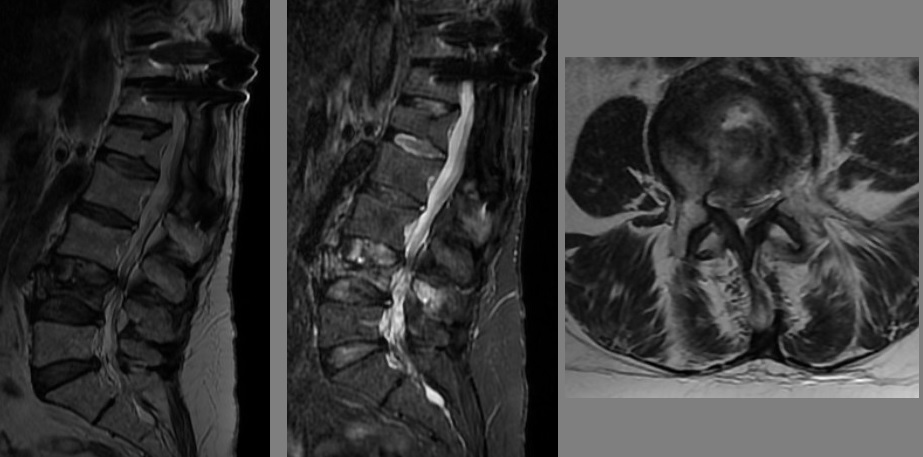
Figure 1: MRI examinations show a burst fracture in the acute/subacute phase in the L4 vertebra and significant canal stenosis at this level.
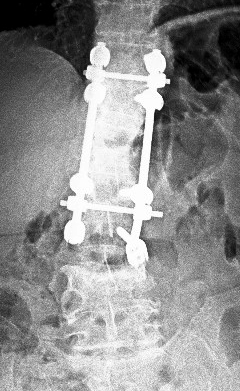
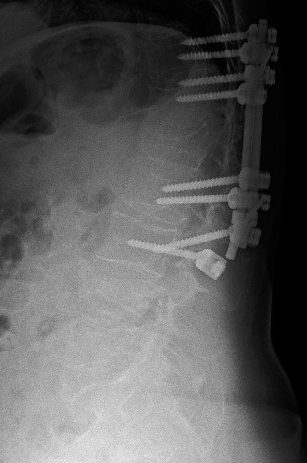
Figure 2: Plain radiographs show the dysfunction of the T11-L3 transpedicular screw system placed for a previous L1 fracture, in addition to the fracture in the L4 vertebra. In the L3 screw, screw pullout likely due to loosening is seen on the right side, and the screw head has disengaged from the rod on the left.

Figure 3: The CT scan shows screw loosening on the right at the L3 level (sclerotic halo around the screw), height loss in the anterior and middle columns of the L4 vertebra, fracture lines extending to the corpus and left pedicle, and significant separation in the facet joints on the left at this level. Other screws belonging to the system are not loosened. There is partial facet fusion at the L2-3 level and complete facet fusion at the levels above.
The patient, who could mobilize with a lumbostat corset, had a good general condition, and her neurological examination was unremarkable except for the old sequelae left hemiparesis. She had severe low back (9/10) and left leg (7/10) pain.
Evaluating her current condition with radiographs and examination findings, it was decided to perform vertebroplasty and epidural injection for pain relief.
Treatment Applied
Vertebroplasty was performed on the patient via the left unipedicular approach under local anesthesia and sedation (6 ml methylmethacrylate). Additionally, facet medial branch blocks and left L3-4 and L4-5 transforaminal epidural injections were also administered.
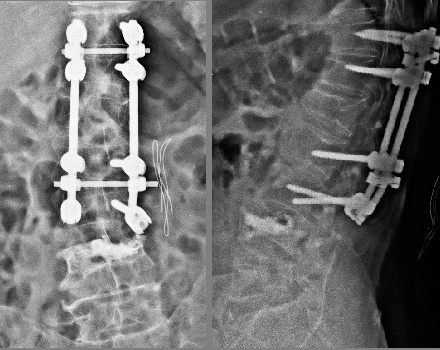
Figure 4: Plain radiographs after L4 vertebroplasty.
The patient described a significant decrease in low back and leg pain (3-4/10) after the procedure. She is mobilized and has no problems in short-term follow-up.
CONCLUSION and COMMENT
It is not uncommon to see fractures at levels adjacent to previously placed instrumentation, especially after trauma. This is because while the levels within the instrumentation system are relatively protected, the vertebrae adjacent to the system (above and below) are levels where stress is concentrated. It is necessary to take this stress concentration and the general condition of the spine into account when planning treatment.
In this patient, the failure in the instrumentation system is a confounding factor in the management of the case. This dysfunction suggests that it may be partly responsible for the symptoms and that it would be appropriate to revise the instrumentation system while treating the L4 fracture, thus making it logical to establish a new system that includes the L4 level.
However, the patient's period before the fall a month ago and the fracture at the L4 level was relatively uneventful. Therefore, considering that the loosening at the lower end of the system was asymptomatic and did not require treatment, it was decided to treat only the L4 fracture and the associated canal stenosis. The fact that the facets at the L2-3 level, where there was loosening, were partially fused and stable, and no gas was seen in the L2-3 disc in the CT examination influenced this decision. Likewise, the L3-4 disc was also quite well preserved. These factors suggested that stabilizing the L4 vertebra would be sufficient, and vertebroplasty was decided upon.
The second difficulty in the patient is that the fracture at the L4 level narrows the canal and the patient has left leg pain in addition to low back pain. If this stenosis had caused a neurological deficit, surgery for canal decompression would have been necessary. However, since there was only pain, it was thought that the problem might consist of temporary root trauma due to acute narrowing of the canal followed by edema, and if radicular pain control is achieved and the vertebra is stabilized with vertebroplasty, there may be no symptoms related to canal stenosis in the long term. For this reason, a transforaminal epidural injection was also applied during vertebroplasty.
The significant decrease in leg pain and its non-recurrence support the correctness of this theory. Of course, this thought could have been wrong, and the leg pain in the patient could have persisted. In this case, the second step planned was to decompress the root under pressure with a minimally invasive decompression.
The alternative to the applied treatment is the revision of the lower end of the dysfunctional instrumentation system, extending the instrumentation system one level below (L5), and providing canal decompression with laminectomy in the same session. It is obvious that such a surgery, which would require general anesthesia, could bring its own problems and future risks.
The treatment performed is an example of the stepwise minimally invasive intervention philosophy that we frequently apply. The cornerstones of this philosophy are to identify the main problem causing the clinical issue and correct the clinical picture with the smallest and least risky intervention possible (if possible, without any intervention), if the applied intervention is not sufficient, to add the next least invasive intervention and follow the patient, and to always save the most invasive and risky interventions for last.