Lumbar Instrument Failure and Solution with Dynamic Stabilization
A 64-year-old female patient was brought in with complaints of severe low back pain, pain in the hips and legs, numbness, cramps, and inability to walk. Her history revealed that she had undergone surgery in the lumbar region three years ago for low back and leg pain, with screw placement. While there was some improvement after this surgery, her condition began to deteriorate again over the last year. It was learned that she had difficulty walking due to the severity of her pain for the last three months and could only move within the house with assistance, and the pain present even at rest increased with movement.
The patient was brought in a wheelchair. Her general condition was good, vital signs were stable, and physical examination was unremarkable except for obesity. Her medical history included lung problems. The neurological examination was normal. She could only walk with a walker due to pain. An incision extending from the lower thoracic region to the sacrum was present, and the lower levels were extremely tender on palpation.
The patient's lumbar MRI from the previous year is shown below.
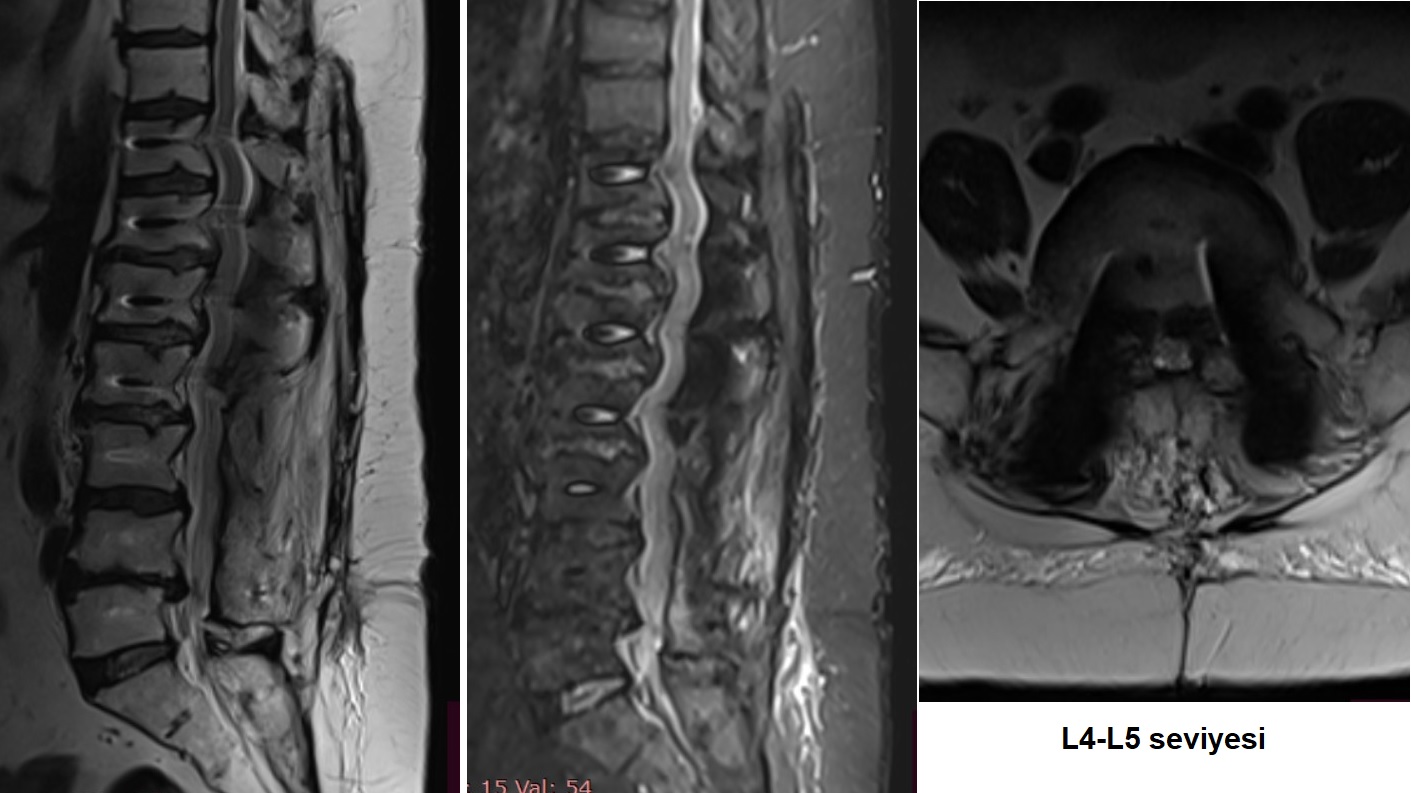
Figure 1: MRI examination performed one year ago showed that the T11-L5 levels were stabilized, there was laminectomy at L2-L4 levels, and stenosis at the L4-5 level. Flattening of the lumbar lordosis was also noted. (MRI quality is low).
In a patient with long-segment (T11-L5) stabilization, hip and leg pain and numbness at rest suggest neural compression due to stenosis in the spinal canal or neural foramina (Although leg cramps can be part of the neurogenic claudication picture, they are not part of the typical sciatica picture, so other causes should also be sought).
Low back pain increasing with movement suggests instability, while severe pain elicited by pressing on the implant in the lower lumbar region supports implant loosening.
Possible diagnoses in this patient are adjacent segment disease (stenosis and/or instability due to accelerated degeneration at levels above T11 and below L5) and implant loosening. The presence of stenosis at the stabilized L4-5 level, while the L5-S1 level is relatively preserved, suggests that fusion did not occur at the L4-5 level and that there might be implant loosening.
Based on these findings, a new MRI and CT scan were requested.
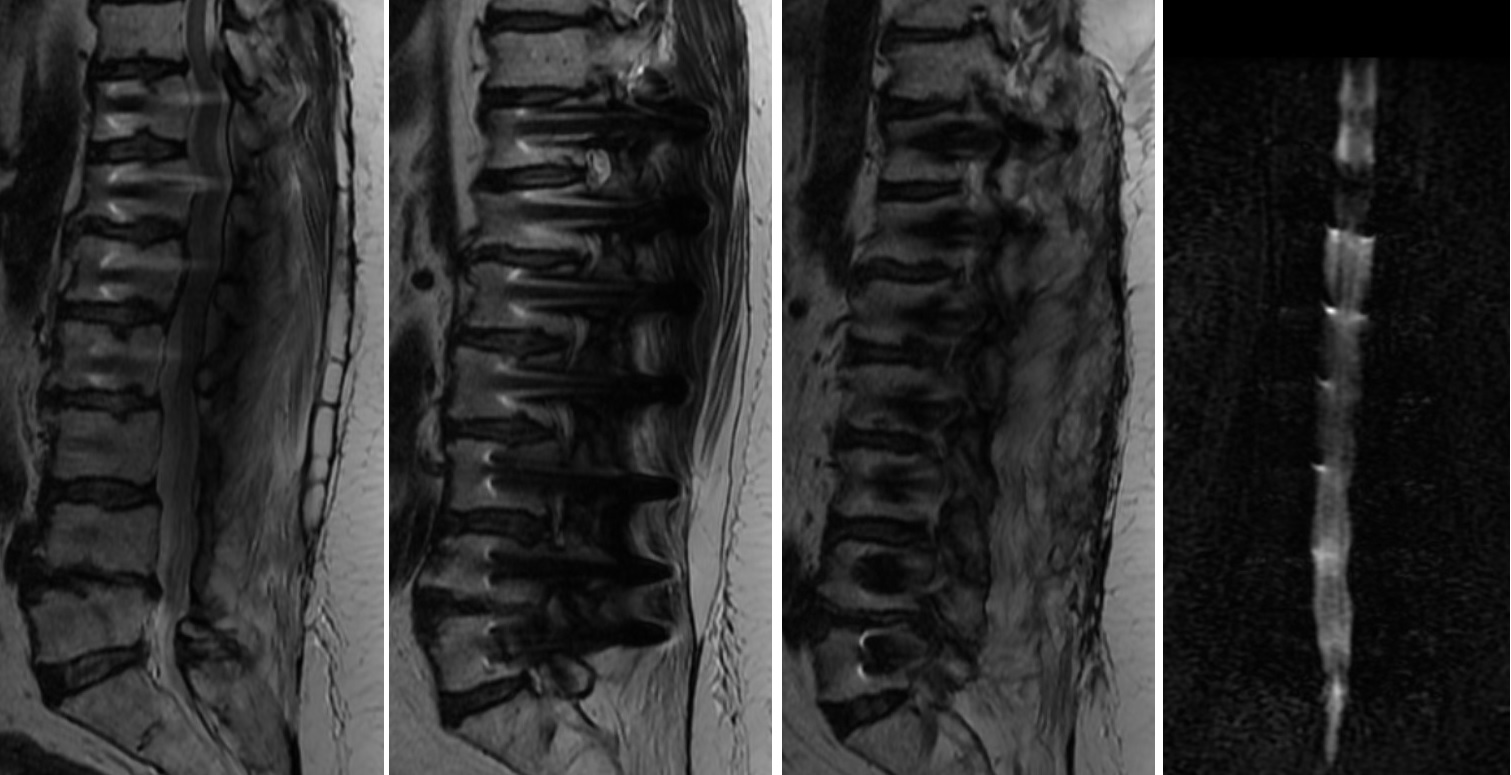
Figure 2: The requested MRI examination shows median, right and left paramedian sections, and MR-myelography. There is no central stenosis at lower levels, while the T10-T11 level is suspicious. However, in paramedian sections, there is suspicion of lateral recess and foramen stenosis at T9-T10, T10-T11, L4-5, and L5-S1 levels. Artifacts from implants prevent an ideal evaluation.

Figure 3: CT examination reveals hypodensity consistent with gas within the T10-T11 and L4-L5 discs and also within the canal behind the L4 body, bilateral loosening in L4 and L5 screws, and foraminal stenosis. Additionally, incomplete facet fusions were observed at the L3-4 and L4-5 levels. No loosening or malposition was detected in other screws.
Following these examinations, detailed analysis of the levels was performed to identify the problematic and symptomatic levels.
T10-T11 level
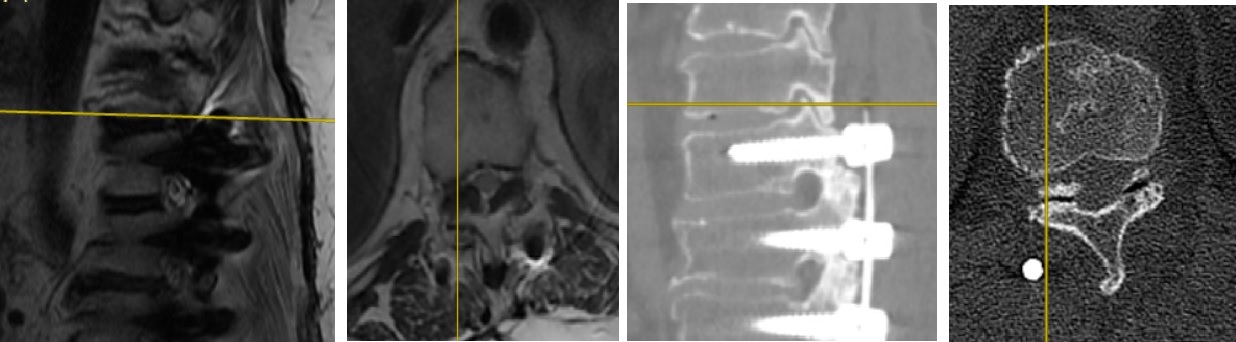
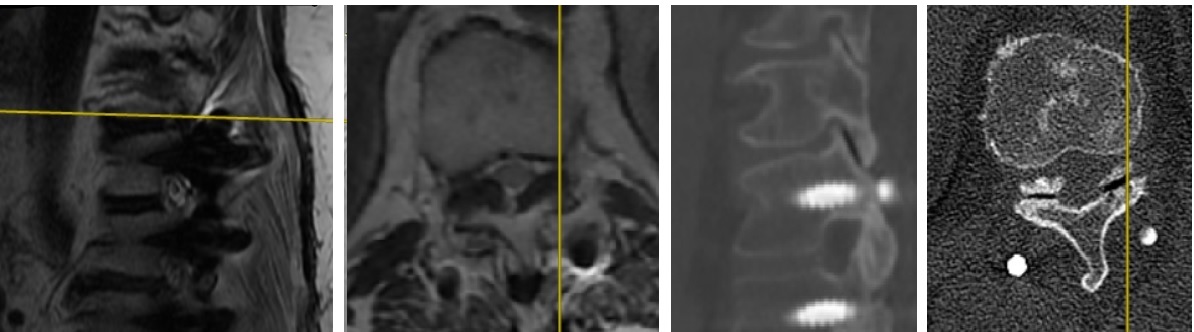
Figure 4: When MRI and CT examinations are combined, accelerated adjacent segment degeneration is seen at the cranial end of the instrumentation system (T10-T11 level). The spinal canal is moderately narrowed due to ligamentum flavum hypertrophy, and gas shadows have formed within the intervertebral disc and facet joints which degenerated due to increased range of motion. Due to decreased lumbar lordosis, the thoracic kyphosis has flattened to maintain balance in the sagittal plane, forcing thoracic vertebrae into retrolisthesis, and consequently, the superior articular processes have narrowed the intervertebral foramina. Similar findings are present more mildly at the T9-T10 level.
L4-L5 level
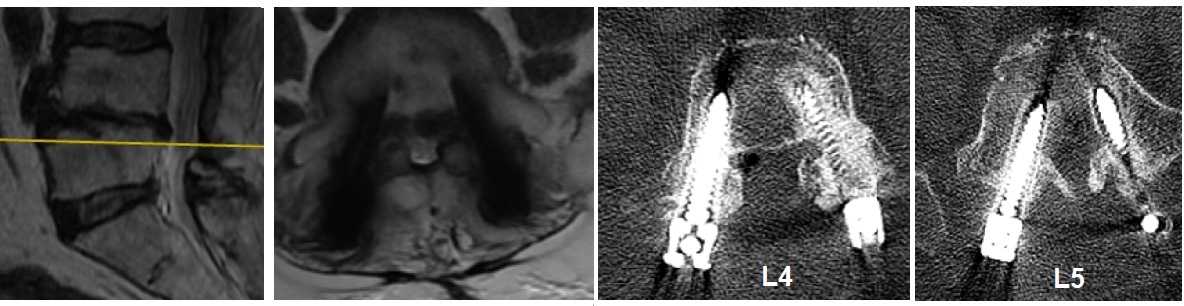
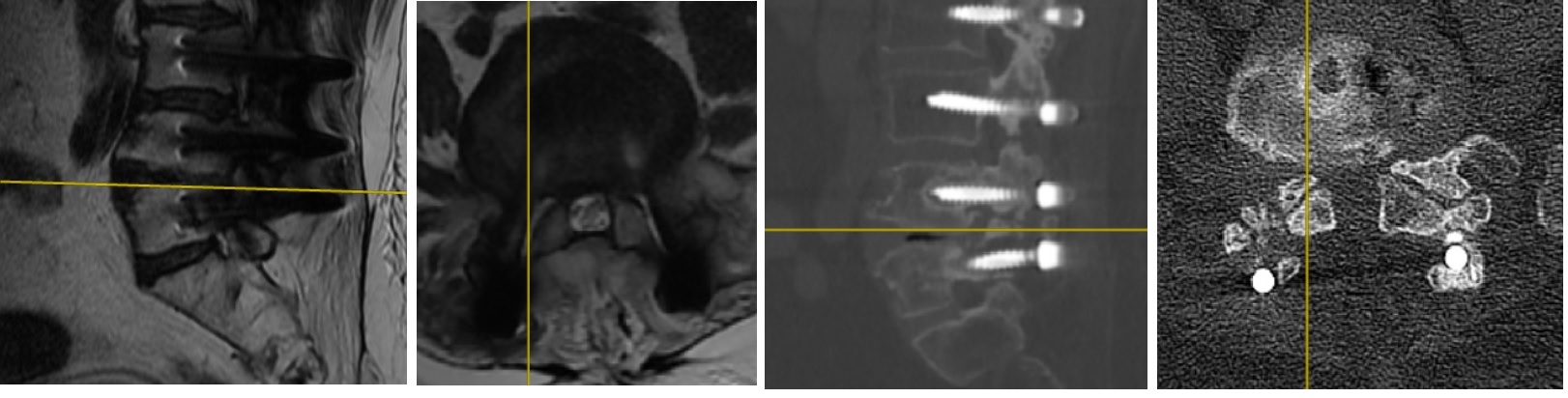
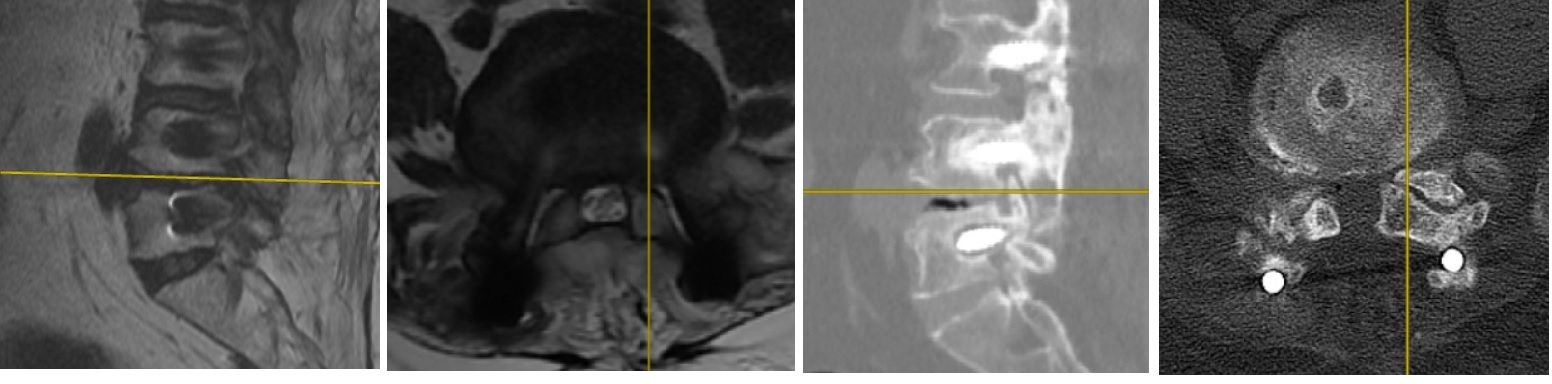
Figure 5: In the central (top row), right foraminal (middle row), and left foraminal (bottom row) images at the L4-5 level, it is seen that the lateral recesses within the canal are narrowed bilaterally, and the bilateral L4-5 foramina are narrowed, more prominently on the left.
L5-S1 level
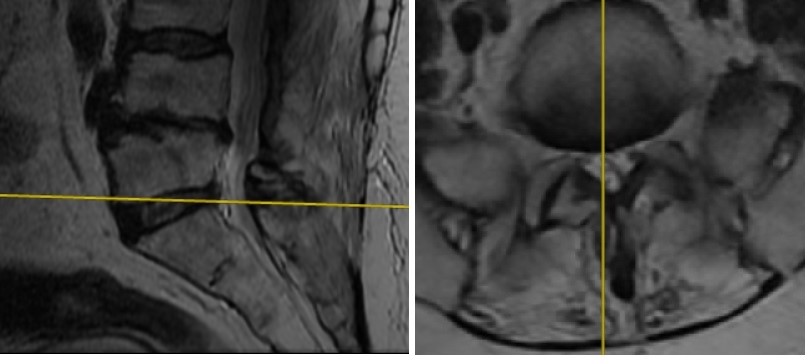
Figure 6: The L5-S1 level is relatively better preserved, and the lateral recesses are open. However, it is observed that the loosened L5 screw on the left has eroded the lower wall of the L5 pedicle, narrowing the foramen (L4-5 images bottom row). The L5-S1 right neural foramen is normal (L4-5 images middle row).
Consequently, adjacent segment degeneration at the upper end (T10-T11), loosening of L4 and L5 screws at the lower end, bilateral lateral recess and foraminal stenosis at L4-5, and foraminal stenosis due to the loosened L5 screw on the left at L5-S1 were detected.
A decision was made to perform revision decompression and stabilization surgery.
SURGERY

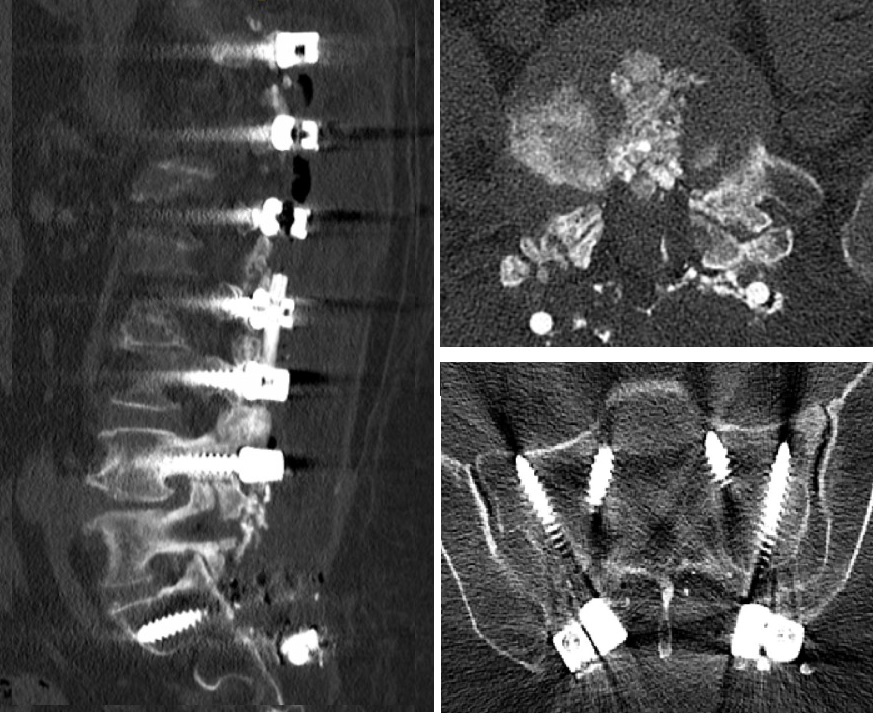
Figure 7: In the surgery, the old incision was opened, and the titanium rods were removed. The L4-5 level was opened, and the intracanal area and foramen exits were decompressed. The disc space was emptied and filled with autogenous bone graft. The loosened L4 and L5 screws were removed. The L4 screws were replaced with thicker ones, while no screw was placed at the L5 level. Screws were placed at the S1 and S2 levels (S1 oriented medially and caudally, S2 screws oriented laterally and cranially). The system was stabilized with PEEK rods extending from L2 screws to S2 screws.
Postoperatively, respiratory distress was observed, which resolved within a day. The patient was mobilized the next day, and there was a significant decrease in her pain complaints. The patient was discharged on the third day but returned on the fifth postoperative day with complaints of serous discharge from the wound. The discharge was stopped with simple suturing, and no other wound problems were observed.
The patient was mobilized in short-term follow-up and is in good condition.
CONCLUSION and COMMENT
The primary problem in the patient was identified as the failure of fusion at the L4-5 level, leading to implant loosening and neural compression due to continued motion. L4-5 was decompressed, and the space was filled with bone graft aiming for interbody fusion. Screws could not be placed in the L5 pedicle, which was severely expanded and damaged due to screw movements, so the procedure was extended to the sacrum. An alternative could have been filling the L5 body with bone cement and placing screws in the L5 pedicles. However, due to the erosion of the lower wall of the L5 pedicle on the left and the presence of foraminal stenosis, this method was not considered safe. The system was stabilized with PEEK rods, establishing a dynamic stabilization that allows partial movement. It is thought that this system will provide a more physiological stabilization compared to rigid stabilization by working in harmony with the relatively preserved L5-S1 disc level, that the L4-5 disc level will proceed to fusion as targeted since it bears load, and that the movement of the L5-S1 disc will be partially preserved. Since dynamic systems bear continuous load, there is a risk of screw loosening. This risk was attempted to be reduced by placing 4 screws in the sacrum. An alternative could have been supporting the system with iliac screws. Loosening of the sacral screws in follow-ups is a possibility. In this case, after fusion is completed at the L4-5 level, the sacral screws can be removed, and the L5-S1 disc level can be made mobile again.
Since it was observed that facet fusion was not completed at the L3-4 level, the PEEK rod was connected to the L2 level to strengthen the existing system, and the screws between T11-L1 were left empty to avoid adding extra stress to the thoracolumbar junction. The reason for not removing these screws is that they do not add extra stress to the spine since they are not connected to the rod, and on the other hand, they offer the possibility of being used in the future if needed in case of an unexpected problem during follow-up.
Although our patient also has adjacent segment disease at the cranial end of the system, this was not intervened. This is because there are no objective neural compression symptoms related to the canal and foramen narrowing here. Nevertheless, there is a possibility that the stress here could affect the thoracolumbar junction and create symptoms (=Thoracolumbar junction syndrome, =Maigne syndrome). In this syndrome, pain can radiate to the iliac crests via the cluneal nerves and mimic lower lumbar symptoms. If such a situation is thought to occur during follow-up, additional intervention may be required.
In summary, our patient is an example of the problems (adjacent segment degeneration and construct failure) that can be seen following long-segment lumbar stabilization performed without restoring lumbar lordosis, and an attempt was made to treat the causes of the current symptomatology with minimally invasive solutions and dynamic stabilization. The alternative is to perform the necessary decompressions and osteotomies to provide lordosis following the measurement of pelvic parameters to ensure global sagittal balance and to establish a fusion system that extends the system further up (lower thoracic) and further down (probably pelvis). Our opinion is that minimally invasive approaches and fusionless stabilizations, as applied in this patient, contribute more to the patients' quality of life with lower complication rates.