Os Odontoideum
A 56-year-old female patient presented with complaints of long-standing upper neck pain and occasional feelings of electric shock and numbness radiating to her arms. Neurological examination revealed no pathological findings other than hyperactive deep tendon reflexes. It was found that the patient had been examined 12 years ago for right arm pain, diagnosed with C6-C7 disc herniation, and underwent anterior discectomy and fusion surgery.
In the magnetic resonance imaging (MRI) from that date, in addition to the disc herniation at the C6-C7 level, it was seen that the dens had separated as a distinct bone (= os odontoideum). It was determined that the patient's arm pain resolved after the surgery, but the long-standing neck pain persisted, and she was unaware of this pathological condition in her C2 vertebra.
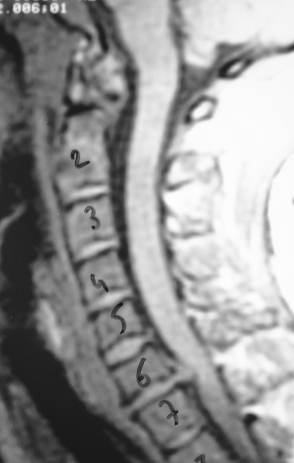
Figure 1: In the cervical MRI dated 1999 (taken 12 years ago), a disc herniation is seen at the C6-C7 level, and at the same time, the dens is seen to have separated from the C2 body to become a separate bone (= os odontoideum).
Cervical MRI, CT, and plain radiographs in flexion/extension postures were performed on the patient. These examinations showed that the dens had separated from the C2 body, becoming a separate bone fragment with sclerotic edges (=os odontoideum) and displaced cranially and slightly posteriorly. The C1 (atlas) anterior arch had shifted slightly backward to the location where the dens should be. CT scans showed that the os odontoideum was fused to the anterior arch of the atlas, and functional radiographs showed that the atlas shifted slightly backward.
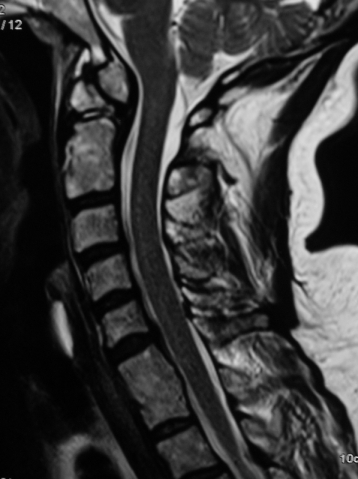
Figure 2: In the T2-weighted cervical MRI, it is seen that the dens has separated from the C2 body and displaced cranially and slightly posteriorly, while the C1 (atlas) anterior arch has shifted slightly backward to the location where the dens should be. C6 and C7 vertebral bodies are fused, and there is bulging in the C5-C6 disc.
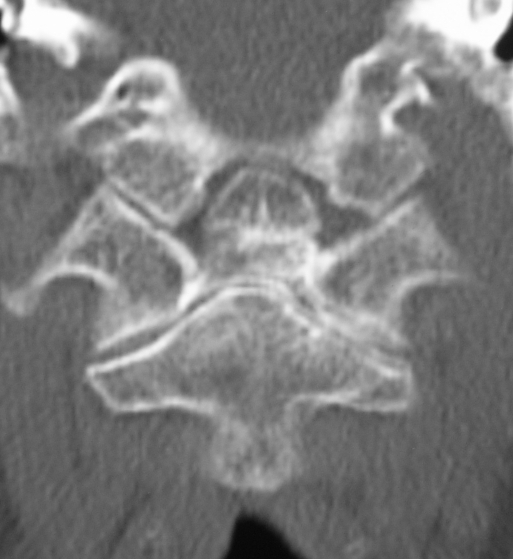
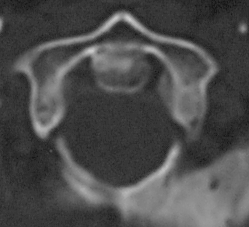
Figure 3: In the coronal CT section (left), the dens is seen to have separated from the C2 body as a separate bone with sclerotic edges (=os odontoideum). In the axial CT section (right), the os odontoideum is seen to be fused to the anterior arch of the atlas.
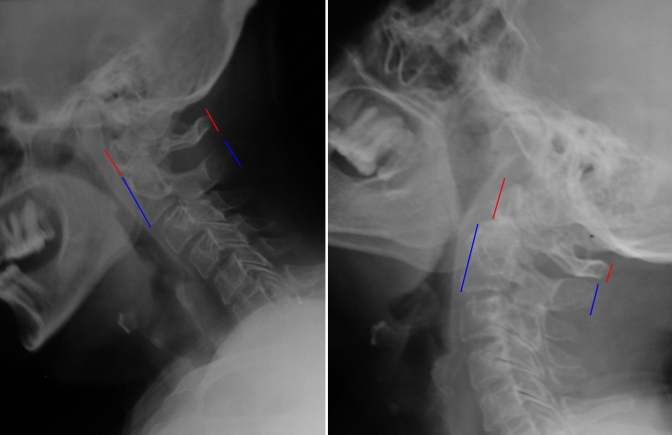
Figure 4: Flexion/extension radiographs show that the atlas shifts slightly backward in extension (=atlantoaxial instability). Additionally, there are slight shifts at the C3-C4 and C4-C5 levels in the flexion radiograph.
The upper neck pain that had been present for many years and was unresponsive to conservative treatments, along with intermittent symptoms of numbness and electric shock sensations in the arms, were consistent with the radiologically detected findings of atlantoaxial instability. This information and findings were shared with the patient, and the benefits and risks of fixation surgery were discussed mutually. A decision for atlantoaxial fixation was made.
Surgery
C1-C2 segmental fixation (Goel-Harms technique) was performed via a posterior approach. Bilateral C1 lateral mass screws and C2 intralaminar screws were used. Autogenous grafts taken from the iliac crest were laid in the C1-C2 interlaminar area to achieve fusion.
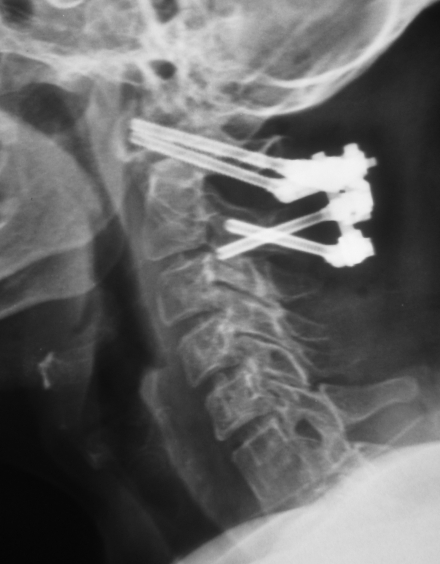
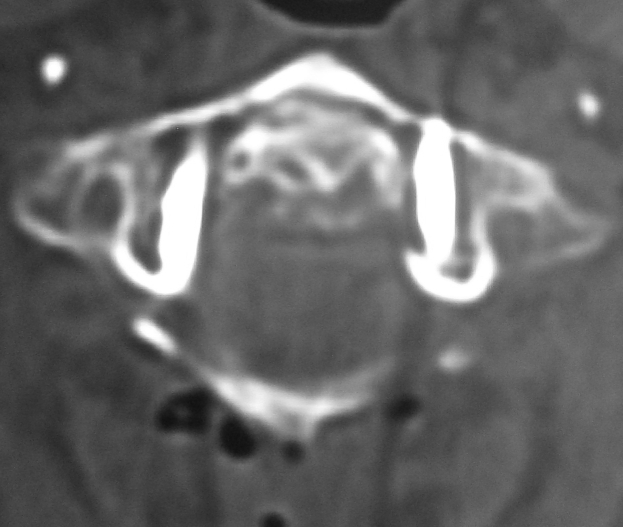

Figure 5: Postoperative plain radiograph and CT examinations show the stabilization system at the C1-C2 level. Lateral mass screws were used at the C1 level (middle image), and intralaminar screws were used at the C2 level (rightmost image) because the pedicles were not suitable for screw application (high-riding vertebral artery).
Follow-up
No complications developed during or after surgery. From the early period, the patient stated that the complaints of numbness and electric shock in her arms had resolved. Neck pain continued, although decreased. The patient is in the 9th postoperative month and is under our follow-up for both the instrumentation system and fusion, as well as minimal degenerative listhesis between C3-C5.
Comment
Os odontoideum has been reported at all ages between the 1st and 6th decades. Atlantoaxial instability is common in these patients. Surgery is necessary in symptomatic cases with radiologically documented atlantoaxial instability. C1-C2 posterior segmental fixation (Goel-Harms technique) is an effective method in these cases.